Resilience is the backbone of emergency management. The nation’s ability to weather storms and disasters without experiencing loss significantly reduces our risk. The Federal Emergency Management Agency (FEMA) developed this guide in collaboration with, and support from, the U.S. Department of Health and Human Services’ (HHS) Office of the Assistant Secretary for Preparedness and Response (ASPR) and other partners to meet, in part, the requirements of Section 1208 of the Disaster Recovery Reform Act of 2018. This article informs local jurisdictions, first responders, utility companies, and healthcare facilities on:
- Healthcare facility preparedness standards and challenges;
- Ways to integrate emergency preparedness efforts throughout the whole community; and
- Methods for prioritizing assistance to hospitals, nursing homes, and other long-term care facilities during power outages.
Background
Across the nation, in every community, there are individuals in hospitals, nursing homes, and other long-term care facilities dependent on power for their well-being. A wide range of facilities provide care in the United States. A portion of these facilities fall within the seventeen provider and supplier types regulated by states and the Centers for Medicare and Medicaid Services (CMS), including emergency preparedness regulations. The seventeen provider and supplier types identified by CMS are:
- Religious Nonmedical Health Care Institutions,
- Ambulatory Surgical Centers,
- Hospices,
- Psychiatric Residential Treatment Facilities,
- Programs for All-Inclusive Care for the Elderly,
- Hospitals,
- Transplant Centers,
- Long-term Care Facilities,
- Intermediate Care Facilities for Individuals with Intellectual Disabilities,
- Home Health Agencies,
- Comprehensive Outpatient Rehabilitation Facilities,
- Critical Access Hospitals,
- Providers of Outpatient Physical Therapy and Speech-Language Pathology Services,
- Community Mental Health Centers,
- Organ Procurement Organizations,
- Rural Health Clinics and Federally Qualified Health Centers, and
- End-Stage Renal Disease Facilities
A portion (e.g., assisted living facilities, board and care homes, individuals living at home) are not regulated by CMS but still may have electrically dependent residents. Individuals rely on electricity in several ways. Patients of some facilities, such as hospitals, receive acute medical care that relies on electricity. Other individuals with access and functional needs or chronic health conditions rely on power-dependent durable medical equipment (e.g., powered wheelchairs, ventilators), but may reside in an assisted living facility, board and care home, or their own home. Individuals also may have an implanted cardiac device that must be plugged in to recharge. Some individuals cannot regulate their own body temperatures and are vulnerable to a lack of environmental controls, such as air conditioning.
Healthcare facility buildings also rely on electricity for many operations, including lighting, security systems, fire alarm and egress systems, environmental controls (e.g., air conditioning), electronic health records, and an array of electricity-dependent durable medical equipment and devices to provide care. In addition, resident populations require daily support (food, water, and transportation), all of which require an intact electrical supply. These requirements, and the fact that healthcare facilities generally cannot temporarily suspend operations, make healthcare facilities uniquely susceptible to power outages. Without power, facilities may require evacuation, and evacuation carries significant dangers for specific populations such as those with access and functional needs.
All levels of government and the private sector have long recognized the importance of power at healthcare facilities, and yet challenges occur with almost every major disaster. One of the more frequent response stabilization activities is providing temporary power (e.g., generator) support for hospitals and skilled nursing facilities. This phenomenon recurs for a multitude of reasons, and although healthcare facility leaders are responsible for preparing their facilities for power outages in accordance with applicable regulation, the whole community (to include all levels of government and utility operators) can help improve these facilities’ resilience to power outages.
Healthcare Facility Preparedness
Resilience to power outages begins with the facility and its leadership. Facilities that prepare and plan for the unexpected will be less likely to have catastrophic failures and will be able to request and receive temporary assets faster if needed.
This section discusses challenges to maintaining healthcare operations during a power outage, good practices to increasing facility resilience, regulations requiring healthcare emergency preparedness, and areas of consideration with regards to regulations.
Challenges To Healthcare Resilience During Power Outages
Generating standby power during a power outage is a complex undertaking. Numerous challenges can impact the ability of a facility to provide adequate emergency power.
Increased Facility Reliance on Electrical Power
The electrical dependence of an organization increases as its functions become more complex. At the most basic level, standard building operations such as lighting, security systems, and elevators require electricity. Fire alarm and suppression systems are essential and require not only electricity but backup power supplies.
Since many healthcare facilities have resident populations, hygiene and feeding capabilities are also part of the electrical demand. Environmental controls, such as heating and air conditioning, are very important as patient populations are often susceptible to temperature changes. At higher levels of care, other important electrical loads include life-support systems, monitoring capabilities, diagnostic capabilities (e.g., radiology, laboratory), blood banking and transfusion services, morgue operations, and pharmaceutical and other supply storage.
Regulations do not mandate that emergency standby power generation be available for all existing functions. Regulations such as 1 FR 63859: Medicare and Medicaid Programs: Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers require emergency standby power to particularly sensitive areas in hospitals, including operating rooms and critical care units where even a momentary interruption in power could mean life or death for an individual patient.
Scientific and technological advancements have both improved the care patients receive and increased healthcare facilities’ reliance on electricity. One example of increased electrical load in healthcare facilities relates to electronic health records and other computer-controlled systems (e.g., voice over internet phones). Electronic health records are now found in most major healthcare facilities and are critical to the care delivered. In 2015, 84 percent of all non-federal acute care hospitals had adopted a Basic Electronic Health Record with clinician notes. A patient’s clinical status, medications, treatments, and other important parameters are all stored and ordered through these systems.
Given the increase in reliance on computer-controlled systems, some facilities have complex server rooms that require their own environmentally controlled support systems.
Standby Power Generation Issues
In the event of power interruption, emergency power supply systems provide emergency standby power to facilities. These systems are susceptible to design, capacity, and maintenance issues.
Design Issues
Emergency power supply systems are complex. When evaluating standby power capabilities, consider that each component of the system can have independent vulnerabilities. Example design issues include:
- System components (e.g., fuel pumps) located in a position where they are vulnerable to hazard impacts, such as flooding or wind.
- Generator system components can include the motor and alternator, transfer switches, electrical lines, battery-starting mechanisms, fuel storage, fuel pump, fuel pump, and exhaust.
- System components not designed to withstand hazard impacts. For example, battery-starting mechanisms and exhaust stacks not secured properly to withstand earthquake impacts.
- System components and required transfer switch not appropriately installed to safely remove the facility from the grid to emergency backup power and vice versa when the power is restored.
- Untested components impacting a facility’s ability to operate, for example:
- An organization moving into a new facility and not discovering that the fuel pump for the generator was not on backup power; and
- A new facility discovering in an emergency that red outlets (a standard indicator of outlets connected to emergency backup power) are not connected.
Capacity Issues
Emergency power supply systems have a maximum electrical load that they can carry. Few facilities, especially large ones, have full redundancy of power for their total operating capacity supplied through the emergency standby generator capability. Facility administrators and emergency managers should have a detailed account of which systems are and are not intended to draw on the backup power supply.
Air conditioning systems are often not connected to backup power. Air conditioning consumes a tremendous amount of electricity. By some estimates, for the average facility, adding air conditioning to the backup electrical load will approximately double the required generator support needed. However, in some climates, lack of air conditioning is a serious threat to patient populations, particularly those with conditions that affect their ability to regulate body temperature.
A number of other systems also may not be covered by backup power:
- Environmental control for server rooms
- Diagnostic equipment including radiology
- Morgue
- Lab
- Blood bank, transfusions service, and human tissue storage
- Food preparation areas
- Elevators
- Pharmacy/floor prescription dispensaries.
Additionally, many facilities do not have enough generator capacity to continue supplying the facility in the event of a mechanical generator failure (i.e., if the facility has one generator down for repair, the remaining generators are not able to supply the usual power demand fully).
Generator Loads
The load on a generator is determined by the various power-consuming devices attached to the emergency power supply system. Generators have a maximum load and a rated load. The rated load is lower and is the load a generator can carry for extended periods.
For any given electrical device, the load it places on a generator will vary. The highest load, the startup load, occurs when a device is turned on. All devices supplied by the generator need to be accounted for in determining the overall load.
Maintenance and Resupply Issues
Even with proper preventative maintenance, mechanical failure of standby generators occurs, requiring special expertise and sometimes difficult-to-obtain critical components. Additionally, generators require a constant supply of fuel. While fuel can and often is required to be stored on-site, fuel can degrade if stored for lengthy periods. Post-impact road conditions and availability of relevant resources (e.g., specialized repair personnel, critical components, fuel) all impact generator operations.
Good Practices To Overcome Challenges
A healthcare facility can take multiple measures to improve the resilience of its standby power operations. Good practices to consider are listed below.
Systems Analysis
Facilities should undertake a vulnerability assessment of their standby power systems, to include:
- All system components and hazards likely to impact the facility.
- A detailed accounting of what electrical devices are and are not supplied by the backup power.
- The portions of the facility that will be supplied with standby power during a power interruption, as well as the portions that will not.
- A list of backup requirements from all licensing and accreditation agencies.
- A critical component – a clear understanding of fuel consumption rates while generators are on their rated load, and a conservative estimate of when refueling will be necessary.
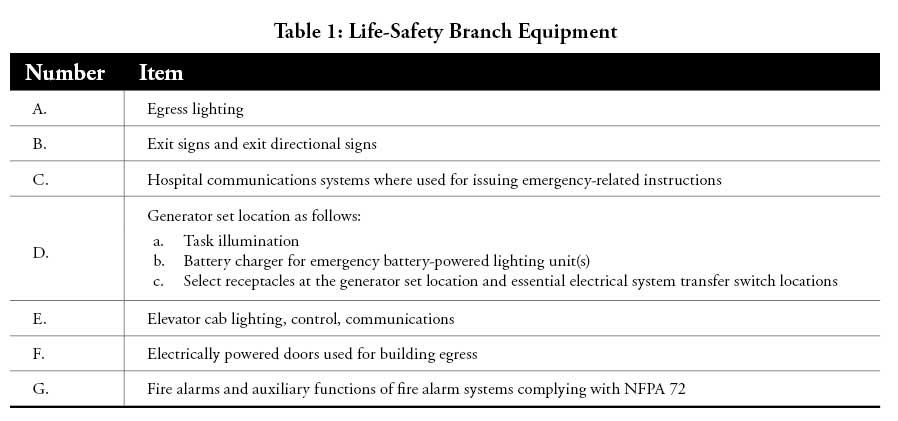
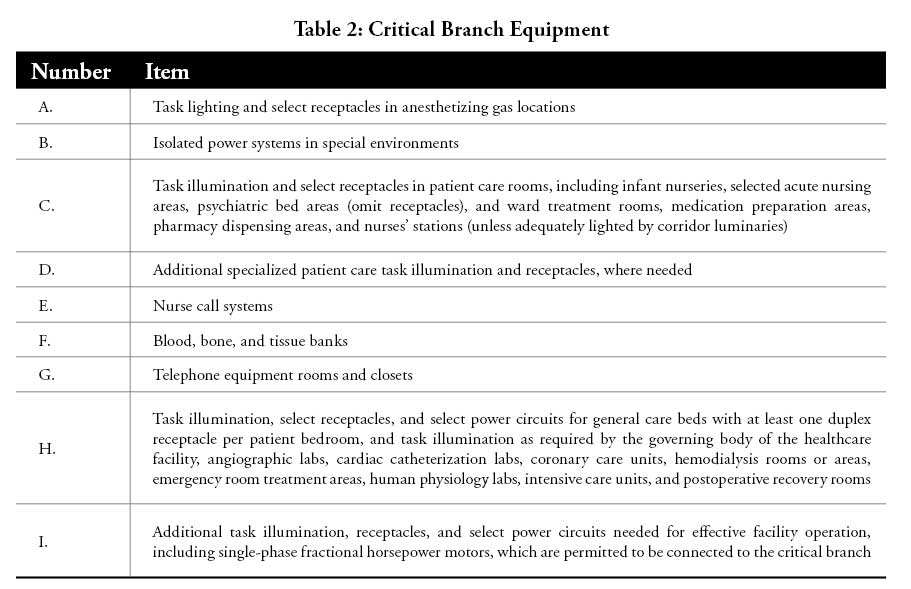
- A load-shedding scheme in which less vital systems are powered down (load shed) to provide power to more critical systems. Appendix A outlines the three branches within an emergency distribution system (i.e., life safety, critical, equipment), which can be a method for facilities to assess the most critical functions that need to remain powered by a diminished emergency power supply.
- An advanced lifecycle analysis in which individual components are evaluated based upon life expectancy. In this manner, predicted replacement schemes can be developed.
A template assessment survey can be found at https://www.poweredforpatients.org/resources/reference-materials/.
Generator Maintenance
Generator maintenance is a complex topic, largely beyond the scope of this guide. However, general good practices include regular servicing, regular load tests to gauge performance, and taking steps to preserve the on-site fuel supply and prevent its degradation.
Some facilities, including hospitals and skilled nursing facilities, are required by regulation to test their generators regularly. These regular tests provide healthcare facilities and local emergency managers an opportunity to complete an assessment during this process. Detailed information on generator maintenance can be found in National Fire Protection Association 110: Standard for Emergency and Standby Power Systems.
Disconnect test
Some facilities test their standby power systems by completely disconnecting from the grid. This test accurately identifies areas that are not clearly supplied by backup power and provides an effective simulation of a power outage. NOTE: A disconnect test has associated challenges and is best conducted with extensive preparations.
Vendor Supplier
Many inoperable emergency power supply systems require repair from an outside vendor. Evaluate vendors for maintenance and fuel for their ability to respond post-impact, especially when transportation routes may be affected. Additionally, consider obligations the vendors may have to other organizations during an incident to ensure they can fully support all customers.
U.S. Army Corps of Engineers (USACE) Emergency Power Facility Assessment Tool (EPFAT)
Following a disaster, it can take USACE many hours, possibly days, to deploy assessment teams to all of the impacted critical public facilities. However, USACE provides a free web-based self- assessment tool at https://epfat.usace.army.mil/ that permits facilities to input, store, and update standby power data before a disaster, which expedites the process if additional generator power from FEMA’s temporary power assets is ever required for a facility. By some estimates, it can reduce the time to establishing additional standby power by up to 30 percent.
Uninterruptible Power Supply (UPS) Systems
Some electronic devices are very sensitive, and even the brief time to switch to backup power can causes malfunctions in equipment (e.g., reboot). UPS systems provide continuous (uninterruptible) power, often for brief periods, and typically supply critical equipment that can be adversely affected by even momentary power outages. Consider UPS systems for particularly sensitive areas (e.g., interventional cardiology).
Generator Quick-Connect Tap Boxes
Even if a facility believes its capabilities are enough for anticipated loads, pre-establishing generator quick-connect tap boxes, also known as generator inlet boxes or docking stations, will help if generators fail or additional power is ultimately needed. Generator quick- connect tap boxes provide a permanent connection point for temporary mobile power. Establish pre-determined areas to place external generators and their fuel supply.
Remote Monitoring
Some systems permit remote monitoring devices. These devices provide a constant status of generator function and early warning of malfunction. With advance warning of a potential failure, deploying government and private sector resources to repair a failing generator can be accelerated. Additionally, if the threatened emergency power supply system cannot be repaired, an early warning of pending failure can give government officials a significant head start and reduce the amount of time needed to deploy temporary generators to replace the failing ones.
The N+1 Principle
N+1 is a strategy providing redundancy to safeguard against a single component failure. In N+1 terminology, “N” stands for the minimum number of devices, such as modules, power sources, and pumps, required to perform the intended function. “N+1” stands for the minimum plus one redundant unit. For example, one large generator may supply critical loads in a building.
However, when called upon, a simple failure will prevent it from operating when needed. Instead, a strategy involving two smaller generators to supply the load, with a third generator of equal size in parallel, provides N+1 redundancy. This strategy also allows a facility to take single units offline for preventative maintenance without sacrificing operations protection.
Overview Of Utility Power Transmission And Distribution Systems
Understanding the basics of utility and temporary power, and its limitations, is important when interfacing with utility companies, vendors, and facility engineers. The below information is from FEMA P-1019: Emergency Power Systems for Critical Facilities: A Best Practices Approach to Improving Reliability.
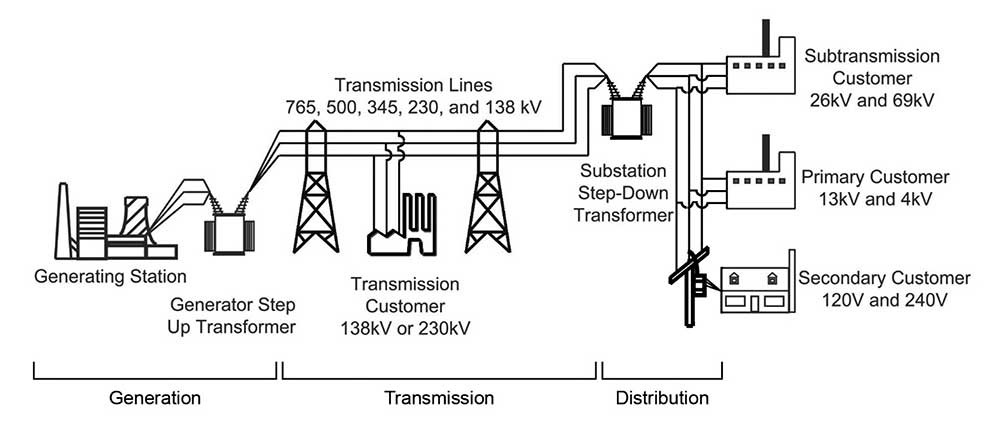
Two basic systems, referred to as transmission and distribution, carry electrical power supplied by utilities from the point of generation to the end-user (see figure 1). The transmission system is the backbone of the utility grid and carries power at the wholesale level. Utility power plants connect directly to this backbone to transport power to local distribution systems and then on to the user. Transmission lines, which operate at very high voltages that range between 69,000 and 765,000 volts, carry electricity to distribution substations. Distribution lines then disperse the power to commercial, industrial, and residential customers. At the boundaries of utility coverage areas, the transmission lines connect to transmission systems of adjoining utilities.
Failures of Transmission Systems
Like the inertia of a large oceangoing vessel moving at top speed, the collective inertial energy of the generators and turbines at each power plant on the utility grid stabilizes the transmission system. This is due to the enormous net inertial energy of all the connected sources. As a result, the transmission system can absorb minor disturbances from individual power plants or retail distribution load points with almost no impact to the overall utility system.
Failures of transmission systems are unlikely but have occurred. Rare natural hazard events that spread damage over a wide geographic area have caused failures to transmission systems. When enough damage accumulates, the overall transmission system goes down, taking with it neighboring utilities in a cascading sequence of failures. Automatic protective systems may trip generating stations offline and isolate ties to neighboring utilities as network operators race to protect their systems. Recovering from such a massive outage takes days to restart power plants, reconnect major system elements, and pick up loads from local distribution systems.
Overview Of Temporary Power
Power sources are devices that create (or store) electricity and ancillary equipment needed for power production and storage. The sources include stored energy devices, generators, fuel supplies, and controls for operating them. Power distribution systems deliver power from the power source to the critical equipment. The distribution system consists of switchgear or switchboards, feeders, distribution panels, panelboards, protective devices, and transfer switches.
Emergency Power Sources
In general, critical facilities employ two common methods of providing emergency power: stored energy devices, such as battery and inverter systems, and standby/emergency generators. Facility personnel must properly size, install, and maintain both types to be reliable and effective. Personnel must also supply fuel-fired generators with appropriate fuel from a reliable source.
Stored Energy Devices
Facilities frequently use stored energy devices to provide short-duration emergency power. When used alone, they often are sized to supply loads for 90 minutes, which allows safe egress from the facility. When used in conjunction with standby or emergency generators, facilities often use stored energy systems to supply power only during the time required to start an emergency or standby generator, stabilize its operation, and transfer critical load to the generator.
Emergency and Standby Generators
Emergency and standby generators serve a wide range of applications. Emergency generators consist of an engine (often called a prime mover), a synchronous generator, monitoring equipment, and controls. Generators require cooling to remove heat created by the prime mover and the generator and ventilation for the combustion air required by the prime mover.
Most emergency and standby generators operate on fossil fuels. Fuel delivery systems are critical to the reliability of fuel-fired generators. Selecting the proper fuel source is important, and many factors play into that decision, including generator consumption rates, the availability of fuels, and the ability to replenish the fuel supply after a natural hazard that blocks roads or disrupts infrastructure. Fuel sources for generators are either liquid (i.e., gasoline, diesel) or gas (i.e., propane, natural gas).
Emergency Power Distribution
The emergency power distribution system includes all wiring and equipment between the emergency or alternate power sources and the critical equipment that the sources supply. Upon sensing normal power loss, an automatic transfer switch automatically sends a start signal to the generator and monitors power quality. When the generator produces power within acceptable voltage and frequency limits, the automatic transfer switch automatically switches from normal to emergency power source.
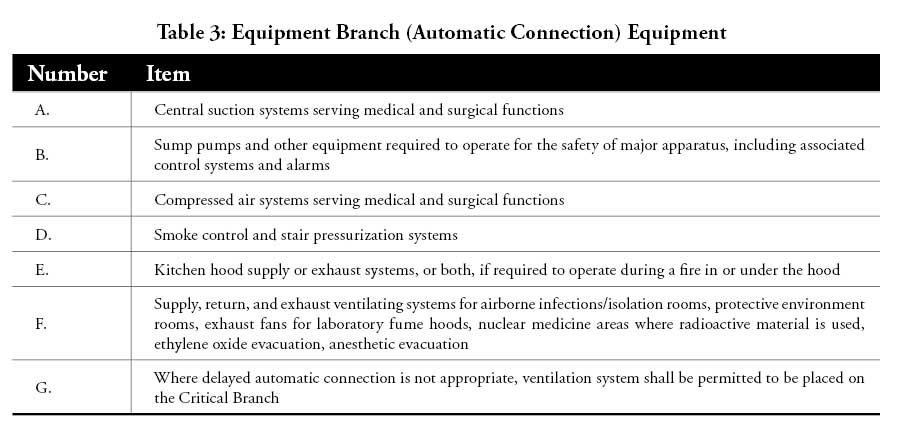
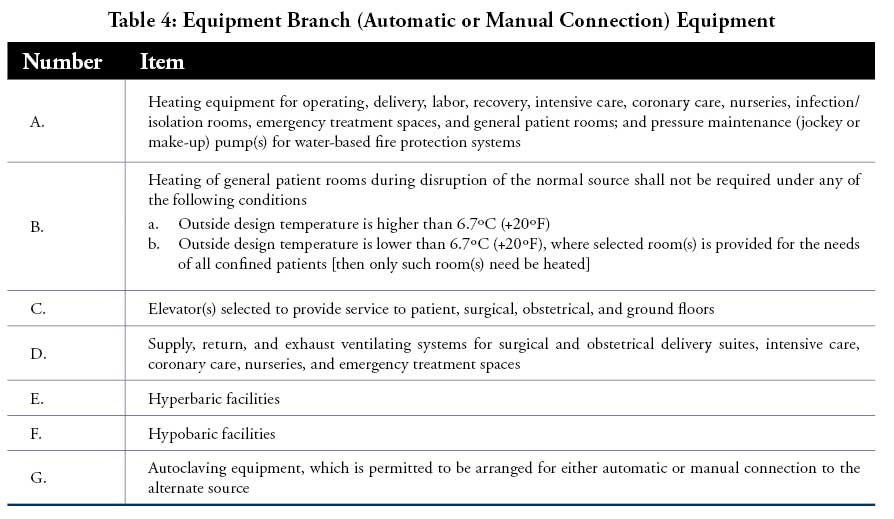
The NFPA 99: Health Care Facilities Code defines three branches within an emergency distribution system:
- Life-safety branch;
- Critical branch; and
- Equipment branch
The life-safety branch is the most important and given highest priority. Table 1–Table 4 detail the equipment that emergency power must support in each branch.
Facilities Not Covered by CMS Regulations
Although the emergency preparedness requirements from CMS apply to a wide variety of facility types, some facilities are not covered.
Non-Medical Care Providing Facilities
Facilities that do not provide skilled nursing and medical care are commonly not subject to Federal and/or state regulatory survey, certification, and oversight. Many of these facilities do not adopt or implement emergency preparedness requirements. These facilities include but are not limited to, assisted living facilities, non-skilled nursing homes, and board and care homes. The populations of these facilities, however, can include individuals with access and functional needs and should be included in community preparedness activities and response priorities.
Small Residential Facilities
The emergency preparedness regulations apply to all 17 provider and supplier types. Some of these facilities, however, may not be subject to all the requirements due to their size and the administrative burden. These facilities include:
- Intermediate Care Facilities for Individuals with Intellectual Disabilities;
- Psychiatric Residential Treatment Facilities;
- Programs of All-Inclusive Care for the Elderly;
- Religious Nonmedical Health Care Institutions; and
- Inpatient Hospices.
Conclusion
A wide variety of natural, technological, and human-caused threats and hazards cause power outages. Patients in hospitals, skilled nursing facilities, and long-term care facilities are at heightened risk during a power outage event. By aiding these facilities to adequately prepare for power outages, coordinating emergency response plans, and prioritizing assistance to these facilities during a power outage, communities can increase their resilience and protect lives.
Resources
CMS-3178-F: Medicare and Medicaid Programs: Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers: Establishes national emergency preparedness requirements for Medicare and Medicaid participating providers and suppliers to plan adequately for both natural and manmade disasters. It also requires providers and suppliers to coordinate with Federal, state, tribal, regional, and local emergency preparedness systems.
(https://www.federalregister.gov/documents/2016/09/16/2016-21404/medicare-and-medicaid-programs-emergency-preparedness-requirements-for-medicare-and-medicaid)
CMS-3277-F: Medicare and Medicaid Programs: Fire Safety Requirements for Certain Healthcare Facilities: Amended the fire safety standards for Medicare and Medicaid participating hospitals, critical access hospitals, long-term care facilities, intermediate-care facilities for individuals with intellectual disabilities, ambulatory surgery centers, hospices which provide inpatient services, religious nonmedical healthcare institutions, and programs of all-inclusive care for the elderly facilities.
(https://www.federalregister.gov/documents/2016/05/04/2016-10043/medicare-and-medicaid-programs-fire-safety-requirements-for-certain-health-care-facilities)
NFPA 99 – Health Care Facilities Code: Establishes criteria for levels of healthcare services or systems based on risk to the patients, staff, or visitors in healthcare facilities to minimize the hazards of fire, explosion, and electricity.
(https://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=99)
NFPA 101 – Life Safety Code: The most widely used source for strategies to protect people based on building construction, protection, and occupancy features that minimize the effects of fire and related hazards.
(https://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=101)
NFPA 110 – Standard for Emergency and Standby Power Systems: Covers performance requirements for emergency and standby power systems providing an alternate source of electrical power in buildings and facilities in the event that normal electrical power source fails.
(https://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=110)
International Building Code: The minimum requirements to safeguard the public health, safety, and general welfare of occupants of new and existing buildings.
(https://www.iccsafe.org/codes-tech-support/codes/the-i-codes/)
FEMA P-1019: Emergency Power Systems for Critical Facilities: A Best Practices Approach to Improving Reliability: Guidance on the design and operation of emergency power systems in critical facilities so that they will be able to remain operational for extended periods, as needed.
(https://www.fema.gov/media-library/assets/documents/101996)
References
1. Office of the National Coordinator for Health Information Technology. “Non-Federal Acute Care Hospital Electronic Health Record Adoption,.” Health IT Quick-Stat #47. https://dashboard.healthit.gov/quickstats/pages/FIG-Hospital-EHR-Adoption.php.













Find Us on Socials